Female Fertility
Testing
"I generally think that if you are under the age of 35 and you've been trying regularly for 12 months, that's a good time to seek help."
– Dr Ying Li
Table of Contents
How will my age affect my chances of falling pregnant?
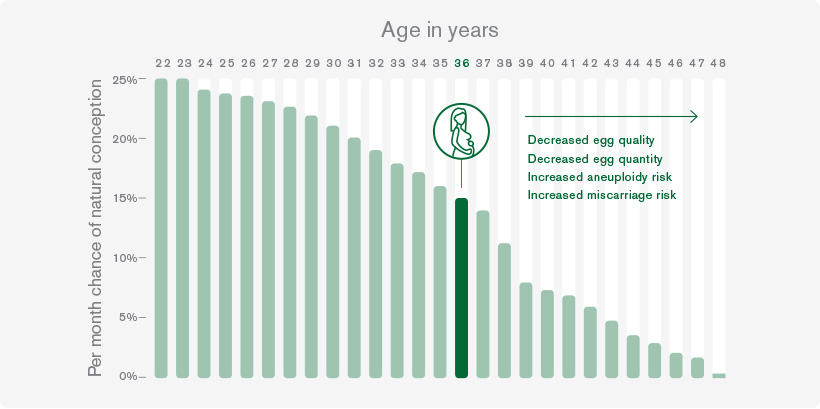
Female fertility declines significantly with age, peaking at 22 and gradually decreasing thereafter. By around 33, the decline accelerates, impacting ovulation and egg health. Ageing eggs can lead to sporadic conception failures and eventual sterility, often years before menopause. Notably, women are born with approximately two million eggs, declining to about 300,000 by their first period. Waiting for fertility treatment exacerbates issues, as chances decline rapidly after 35. Research shows couples often delay treatment for over two years, further diminishing chances.
As you can see from this graph below, by age 36, your monthly chances of conception halve, declining to about 14%, then all the way down to around 1% by age 45.
How can ovulation tracking help?
Before jumping into fertility treatment, you may want to consider ovulation tracking as a first step. It’s a simple option that helps you understand your natural fertility and plan when to have sex, to maximise your potential of getting pregnant. Sperm can live at their healthiest inside the female body for 2-5 days, so you’re more likely to conceive when you have intercourse on, or around, 1-2 days before ovulation.
Is my weight a factor?
The main effect of weight on fertility in women is due to a failure to ovulate – anovulation. There are also other more subtle metabolic effects due to elevated insulin. Women with a Body Mass Index (BMI) of 25-30 are 50 per cent more likely to have anovulatory infertility than women with a normal BMI. This rises to 300% for women with a BMI over 30. Unfortunately, IVF success rates may be reduced by as much as 25% in obese patients and 50% in very obese patients.
Being overweight or obese not only reduces your chances of conceiving naturally, but it also means that fertility treatments like IVF are less likely to be successful. During pregnancy, being overweight can also lead to complications including gestational diabetes and an increased risk of miscarriage, stillbirth, birth defects and obstetric complications.
So you may need to consider a diet for conceiving success and to improve your pregnancy health. The good news is that weight loss itself can be an effective fertility treatment and many patients conceive naturally after focusing on their diet and trying to exercise more.
What is Polycystic Ovary Syndrome (PCOS)?
Around 11% of women around the world suffer from PCOS — although it’s often misdiagnosed, or goes undiagnosed, so the numbers are probably higher. The issue arises when mini cysts form on the ovaries, from egg sacs or follicles that refuse to grow and release an egg through ovulation. Instead, they stall — releasing relatively higher male hormones into the blood, and causing a range of health problems.
It’s a complex condition that can be related to elevated cholesterol, an insulin imbalance and unwanted weight gain. (And metabolic shifts can still occur even if you are slim.) But PCOS doesn’t mean that you can’t conceive…
A combination of blood tests can assess your hormone levels; and a pelvic ultrasound can look at your ovaries to see if the cysts or follicles are present. There’s currently no cure for PCOS, but you can successfully manage the syndrome by making changes to your diet and exercise routines and — in some cases, with medical intervention.
If your weight is already in the normal range or losing weight doesn’t help you conceive, there are a range of other treatments on offer to help you such as medication to increase ovulation, hormonal treatments and surgical options. IVF may be needed if there are other factors involved, such as poor sperm quality, so it’s important that you and your partner are assessed together to decide on the best treatment options.
Is endometriosis common?
Yes, it’s a common cause of infertility, affecting at least 10% of women at some point during their menstruating years, all the way up to menopause. It occurs when tissues that normally line your uterus (the endometrium) grow in abnormal places around your pelvis and, more rarely, other parts of your body.
And because growths produce a series of chemical substances (called cytokines or interleukins), ovulation and egg quality may be impaired, sperm may not function so well, and embryos can find it harder to implant. In more severe endometriosis cases, the ovaries and fallopian tubes distort, causing the body to resist or reject sperm altogether.
While women with endometriosis may be diagnosed through an ultrasound, a definitive diagnosis can only be made with a laparoscopy or, less commonly, open surgery. If surgery doesn’t lead to pregnancy, women tend to move straight onto assisted reproduction like IVF.
What are my chances of a miscarriage?
Miscarriages, though heartbreaking, are not uncommon, occurring in approximately 15 to 20% of all pregnancies, often in the first trimester. These rates increase with age, with one in three women who have given birth in their early 30s experiencing miscarriage. Most miscarriages, which occur before 20 weeks, cannot be prevented, often due to foetal abnormalities. While emotionally challenging, most miscarriages are isolated incidents and indicate a functioning reproductive system. However, recurrent miscarriages, experienced by about 5% of women, suggest underlying issues and may require intervention.
What female fertility tests are available?
There are many tests for women — and most of them require a simple blood test.
Consulting Rooms
Level 3, 321 Kent St
Sydney NSW 2000
137 St Johns Rd,
Glebe, NSW 2037
50-52 Gloucester Rd,
Hurstville NSW 2220
Phone and Fax
T: 1300 323 297
F: 02 8212 8944
Our Female Fertility Tests
Anti-Müllerian Hormone (AMH)
Anti-Müllerian is a hormone produced by the ovaries and is often used as a marker of ovarian reserve, which refers to the number and quality of your remaining eggs. AMH levels can provide insights into your fertility potential.
Follicle-stimulating hormone (FSH)
This hormone helps control your menstrual cycle and your production of eggs. Testing your FSH levels helps evaluate your ovarian reserve or egg supply, and it’s usually done on the third day of your menstrual cycle.
Luteinising Hormone (LH)
This hormone is linked to ovarian hormone production and egg maturation. It’s used to test if you are ovulating, and to help measure your ovarian reserve.
Oestradiol
An important form of oestrogen (the primary female sex hormone), oestradiol is used to measure your ovarian function, and it’s usually done on the third day of your menstrual cycle.
Progesterone
Progesterone is the hormone produced by your ovaries when you ovulate. It triggers the endometrial lining of the uterus to thicken, making it a more receptive environment for a fertilised egg. Three weeks after your period, your progesterone levels may be tested — to find out if you’re ovulating.
Prolactin
Probably best known for its role in human milk production, prolactin is also key to our immune system and helps to aid cell growth. A prolactin test can help discover why you’re not menstruating.
TSH/Thyroid antibody
Every cell in your body depends upon thyroid hormones for regulation, and good thyroid function is necessary for fertility. Testing for your Thyroid Stimulating Hormone (TSH) can tell us if you’re in normal range.
Ultrasound scan
An ultrasound helps to check the health of your womb lining (endometrium) — as well as check for fibroids, polyps or ovarian cysts. It may also be used to check that your fallopian tubes are open.
Female Fragile X carrier test
There are some reports that women who carry the gene that can cause Fragile X syndrome in their offspring, can suffer from premature menopause, so a Fragile X test is available for the most common gene size.
